07 Oct 2021 Nutritional Therapy Strategies for Long-COVID – how to help the long haulers!
With the so-called curse of “Long-COVID” estimated to affect a third of people post-infection, the legacy of this virus is set to disrupt populations for years to come. It is still unclear as to why some people experience the virus more, or less, severely, and why prolonged symptoms linger in some but not in others. Inevitably there are still more questions than answers as the studies play catch-up with the reality of people living their lives blighted by persistent symptoms. Dubbed as ‘long-haulers’ these people are now seeking therapeutic strategies to alleviate and support long-COVID symptoms in a bid to get back to full health as quickly as possible.

BANT Fellow and Consultant in genomic medicine at the University of Stirling, Anh Nguyen, walks us through the latest research and nutritional considerations for supporting long-haulers at the intersection where diet, nutrition and eating habits converge on gut health, inflammation, and specific symptoms of long-COVID, such as loss of olfactory senses, fatigue and poor cognition.
by Anh Nguyen, BANT Fellow, University of Stirling, UK
Nutritional Therapy Strategies for Long-COVID – how to help the long haulers!
“Almost 5 months post-COVID I have little to no taste or sense of smell and lack of appetite. I am extremely lethargic throughout the day and everyday tasks seem to be very difficult. I was active and healthy before.” Mona, Birmingham, UK recalled her symptom
Studies estimated that up to one-third of people post-COVID, like Mona, have been suffering from a new disease which can last anywhere between a month to a year, and sometimes beyond this time frame. Scientists named this disease post-acute sequelae of COVID-19 (PASC), or commonly described as “Long-COVID” or “long-haul COVID” by patients. A systematic review of 45 studies1, consisting of 10,000 patients and 84 discrete symptoms, found that nearly three-quarters of patients reported at least one persistent symptom for a mean or median of 2 to 4 months, and some symptoms were reported to persist for as long as 6 to 8 months. Recently, a number of studies have also paid special attention to children with Long-COVID, though, it is not known exactly how many children with COVID will have long-term COVID. A survey on 3,065 British children age between 11 and 17 demonstrated that 14% of children were still experiencing symptoms 15 weeks post-COVID 2. Similarly, a recent report of The UK Office for National Statistics surveyed half a million children with COVID, found that 12.9% and 14.5% of children aged between 2-11 and 12—16 respectively were still experiencing COVID symptoms five weeks after their first infection3. A US study 4 comprising 300 young patients aged 16-30 years, found that more than 50% of them had symptoms that persisted for more than six months.
Why do some patients experience Long COVID—and others do not?
 All humans have 99.9% identical DNA sequences across the estimated 6 billion-letter code (A, T, G, and C) for their genome. Slight differences (0.1%) exist between individuals, making each of us unique. These differences, called genomic variants, occur at specific locations within the DNA. These variants also may hold essential clues about the causes of diseases. Some variants increase the risk of developing diseases, while others may reduce such risk; some may have no effect on disease risk. So, genotypic information can be used to develop personalised interventions in both nutrition and medicine for the prevention or treatment of a certain disease.
All humans have 99.9% identical DNA sequences across the estimated 6 billion-letter code (A, T, G, and C) for their genome. Slight differences (0.1%) exist between individuals, making each of us unique. These differences, called genomic variants, occur at specific locations within the DNA. These variants also may hold essential clues about the causes of diseases. Some variants increase the risk of developing diseases, while others may reduce such risk; some may have no effect on disease risk. So, genotypic information can be used to develop personalised interventions in both nutrition and medicine for the prevention or treatment of a certain disease.
Genetic studies have partly shed light on how the host genetic information can help to target personalised treatment for COVID disease. By analysing a data set of 50,000 hospitalised patients with severe COVID symptoms, a large group of global scientists 5 revealed 13 genetic signatures in strong relation to an elevated risk of severe COVID disease from 4% to 74%. Not all 13 variants were present in every patient. The findings emphasised that the more variants an individual carries, the bigger their risk for severe disease is. To date, it is not exactly known why some patients have long-COVID symptoms, but others do not. Some data shows that remission of symptoms can be related to genetic variations. A study6 published in the Scientific Reports (Nature) journal revealed that the rs1173773 variant on chromosome 5 is strongly associated with remission of symptoms. Patients carrying rs1173773 Allele C had a greater remission of symptoms compared to Allele T carriers: 59%, 54%, and 44% of individuals with CC, CT, TT genotypes, respectively, had remission of symptoms. The results are novel and are not replicated yet. Moreover, diversity in host genomic research should also be taken into consideration. A genome-wide association study7 in 2000 Japanese COVID-19 patients found that many COVID-related genes except DOCK2 overlapped with European populations (Namkoong et al. 2021). Notably, the DOCK2 variant that increased COVID-19 risk was relatively common in East Asians including Japan but very rare in Europeans. The research on host genomics has yielded promising results for personalised medicine, but its application to clinical practice is still in the embryonic stage.
While studies on host genomes in relation to long COVID are currently ongoing, epidemiological studies revealed factors that are associated with the risk of developing long COVID. It is worth noting that women are more likely to have long COVID than men. Moreover, long COVID is significantly associated with increasing age, particularly age 40 and over. Additionally, the REACT findings8 emphasized there is a 3.5% increase in likelihood in each decade of life. Other clinical risk factors are obesity, smoking, and pre-pandemic health conditions (e.g., mental health, asthma).
Seeking the Root Causes of Long-COVID Symptoms
To date mechanism for long-COVID remains unknown. Multiple mechanisms may be responsible for prolonged symptoms in an individual. Scientists believe that long-COVID symptoms might be a consequence of lingering inflammatory process following SARS-CoV-2 infection9. “Inflammation is the body’s immune system’s response to an irritant”, which can be both beneficial and harmful. Once the body is injured by an infection, the immune system immediately brings “an army” of immune cells and factors to surround and protect the site. There may be “viral reservoirs” including RNA and other components from the SARS-CoV-2 virus that persist in the body and keep the immune system being alert like “having a chronic viral infection”. Recent studies have found “viral reservoirs” in multiple organs including the brain, the lung, and the gastrointestinal tract of long-hauliers10-11, which might continuously stimulate systematic inflammation despite confirmation of a negative COVID-test. Previous viral infections such as Ebola and Zika were also not completely clear in the body. Chronic post-viral fatigue is common among those with these infections. Another possible mechanism in relation to COVID-post symptoms is “molecular mimicry”, which may induce autoimmunity12. A component of the virus13 might resemble a component of human tissue. For example, interleukin 7 and histone-lysine N-methyl transferase C are human proteins that are similar to those of SARS-CoV-2. The immune cells with the ability of immunological memory such as T or B cells may autoreactive human tissues with those proteins. Together or alone, such inflammations or other yet unknown mechanisms might affect a variety of body systems and lead to different symptoms among COVID-long-haulers.
Many theories in association with long-COVID have been focusing on immunopathology effects following the SARS-CoV-2 infection. However, few studies pay attention to diet and lifestyle factors that might contribute to this process as well as prevent an ability to recover from long-COVID symptoms. As seen in Figure 1, malnutrition and COVID-induced biological alternations in an individual can contribute to long-COVID symptoms. Post-COVID patients had a high risk of malnutrition14. Alternations in taste and smell well-reported in some people after infection can contribute to low appetite and inadequate dietary intake as well. As a result, they may not get enough micronutrients or macronutrients that are essential to a normal function of body including immune system.
The European Commission15 has officially recognised the importance of certain micronutrients including Copper (Cu), Selenium (Se), Zinc (Zn), Iron (Fe), B vitamins ( B12, B9, B6), Vitamin A, vitamin C, and vitamin D contribute to the normal function of the immune system. To date, studies have paid particular attention to Selenium, Zinc, Vitamin C and Vitamin D due to their potential as antimicrobial therapy against COVID-19. A systematic review and meta-analysis also demonstrated that the sufficient presence of such essential micronutrients in the body is strongly associated with the reduction in the COVID incidences, severe symptoms, and ICU admission16
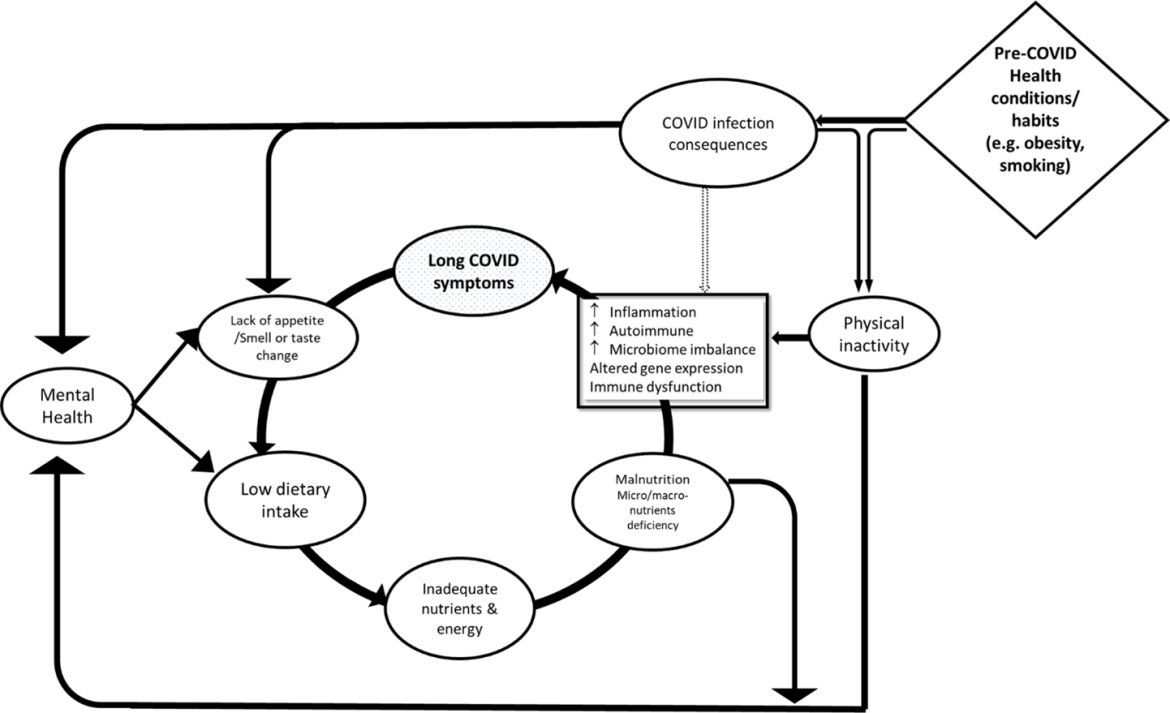 Figure 1: Possible diet and lifestyle factors contributing to prolonged COVID symptoms
Figure 1: Possible diet and lifestyle factors contributing to prolonged COVID symptoms
Other factors such as mental health can get influence low dietary consumption and malnutrition of an individual. Notably, the prevalence of mental health has increased since the pandemic. According to The National Centre for Health Statistics (2020), three times the number of people 17 in the US experienced anxiety or depression between April and June of 2020, compared with the same period of 2019. Other studies in Hong Kong and Italy found that 26% and 55% of people have experienced mental disorders since the pandemic, respectively 18-19. One-third post-COVID patients in the UK developed psychiatric disorders within 24 weeks of infection. Topping the list was anxiety and depression. 20
In addition, restrictive measures during lockdowns or post COVID symptoms consequences may also have affected physical activity of an individual. Not getting enough physical stimulation can contribute to significant drawbacks for health, including the accumulation of body fat, muscle maintenance, increased mental distress, immune dysfunction and increased inflammatory effect. 21, 22 Evidence suggests that there was a significant reduction in physical activities during the lockdown in both adults 23 and children.24 Moreover, sedentary activities such as sitting, and watching/using screens increased during this period. Insufficient physical activity is strongly associated to severe COVID symptoms, ICU admission, deaths as well as other commodities such as obesity, cardiovascular diseases, and hypertension25. Physical activity of individuals with lingering COVID symptoms was influenced up to 6 months post infection.
In addition to COVID-induced biological alternations, malnutrition also can significantly increase the inflammatory process, weaken the immune system, and alter the gut microbiome. Combined, these issues can contribute to a variety of long-COVID symptoms including fatigue, brain fog, lack of taste and smell, weight loss, muscle weakness.
Three nutrition therapy strategies for long-COVID
Given the recent releases of national guidelines on long-COVID, there are no specific recommendations on diet and nutrition for long-hauliers. It is understandable that there is an urgent need for a strategy focusing on diet and nutrition that addresses long COVID symptoms. On CINAHL and PubMed, we conducted a search of literature focusing on long COVID and nutrition until September 2021. Using the Stansfield (2016) three-stage approach26, we had an addition search for grey literature written by experts and published on websites. Inclusion criteria are peer-reviewed articles as well as grey literature written by national-recognised experts such as GPs, BANT/CNHC-registered nutrition practitioners, and dietitians. The John Hopkin Evidence Level and Quality Guide was applied to address the quality of evidence. Studies ranged from trials to reviews28, 37, 41-47. Our findings found that three nutrition therapeutic strategies may support long-COVID.
First strategy
The first strategy aims to lower the hyper-inflammatory process. In this stage, we take a small step to switch from inflammatory food patterns to less inflammatory ones, whilst ensuring the body gets all nutrients it needs. Evidence27 shows post-COVID patients prolonged the inflammatory state up to 2 months since the infection began. Plant-based diets are proven to display anti-inflammatory effects, and may include a variety of vegetables, fruits, nuts, seeds, legumes. Storz (2021) also emphasised that some common long-COVID symptoms such as fatigue, muscle and joint pain, sleep disorders may benefit from plant-based diets28. For example, plant foods can provide dietary fibre that is not typically prevalent in Western diets. Lack of dietary fibre is strongly associated with hyper-inflammatory state-related conditions such as metabolic disorders and autoimmune diseases. In addition, the body does not digest dietary fibre, but instead it is digested by gut microbiome. Gut microbiomes use dietary fibre as a source of food and waste by-products including short-chain fatty acids and other compounds. These by-products help to regulate T-regulatory cells and prevent a hyperactive immune response. Cognition and memory impairments in long-hauliers, commonly described as “brain fog” might be related to post-viral gut dysbiosis. To support this hypothesis, our recent data found that the SARS-CO-V2 virus might affect the gut microbiome in infected patients when compared with healthy people and the altered microbiome could not return to stable levels for up to 6 months. 29 As a result, this may affect the connection between the brain and gut and the digestive function.30
Plant foods also provide good sources of phytochemicals and antioxidants. These “natural agents” can eliminate free radicals and relieve the inflammatory process in relation to potential multiple organ damage caused by long-COVID. For example, quercetin (Que), abundantly found in a variety of vegetables, is a flavonoid with the proven benefits of anti-inflammation. Que also can work as a natural monoamine oxidase inhibitor that supports communications between brain cells by affecting chemical messengers such as serotonin. 31 Increasing intake of plant foods such as fruit and vegetables may increase levels of micronutrients as well.
Following a partial or predominant plant-based diet does not require complete elimination of meat foods from the diet. Animal protein sources such as chicken, egg, and fish are important to get all of the essential amino acids, iron and vitamin B12 that we need. Additionally, oily fish such as sardines and salmon are rich in omega-3 fatty acids DHA and EPA. Omega-3s can remain a normal function of the brain, particularly cognition and memory.
The second strategy
The second strategy aims to connect yourself to the body’s hunger and satiety signals in order to improve appetite and food intake. Choosing healthy foods is not enough for an individual to eat healthily; they also need to consume the right quantity of foods as well. Notably, low appetite and the reduction in food intake have been reported in COVID-19 patients, and now in post-COVID people due to a lack of hunger signals and faster satiation32. The impairments in hunger and satiety sensations may be a consequence of COVID-induced taste and smell disorders. “Mindfulness means focusing on the present moment, while calmly acknowledging and accepting your feelings, thoughts, and bodily sensations”33. Mindful eating based on the fundamental philosophy of mindfulness. Eating mindfully describes an awareness of physical and emotional sensations related to eating non-judgmentally34. The practise of mindful eating can help an individual achieve full attention to sensory perceptions while eating. Moreover, it can increase pleasure eating as well as an awareness of hunger and fullness signals34, 44.
Imagining that we are going to eat an apple. First, we pick up the apple, and pause a little while instead of putting it immediately into the mouth. Holding and looking at the apple can help us to know what we are eating. Then, smelling the apple, biting a small piece and chewing slowly can help us have a full experience of senses associated to the food we are eating. As a result, when you pay attention on purpose at the present moment associated with eating, you can reach full awareness of how senses of sight, smell, taste, and touch interact while eating. Indeed, “When you eat the apple, just concentrate on eating. Being focused and slowing down will allow you to truly savour all the qualities the apple offers: its sweetness, aroma, freshness, juiciness, and crispness” 36
There are some steps to practicing mindful eating that might help long-haulers find their own being while eating
- Select ingredients and prepare your meal.
- Never skip meals
- Sit at the table and focus on eating, no phone or TV interruption
- Wake up all senses while eating by looking at your meal to get your eyes be seen, smelling your meal to get your noses be smelled, chewing slowly to get your ears be heard and to get your tongue be touched.
- Take a small bite at once and focus on your breath in each bite
- Always show gratitude to your meal
The above method does not need to be implemented wholly right away, it can be suggested that mindfulness can first be applied to one meal a day, gradually applying this to more meals throughout the day.
The third strategy
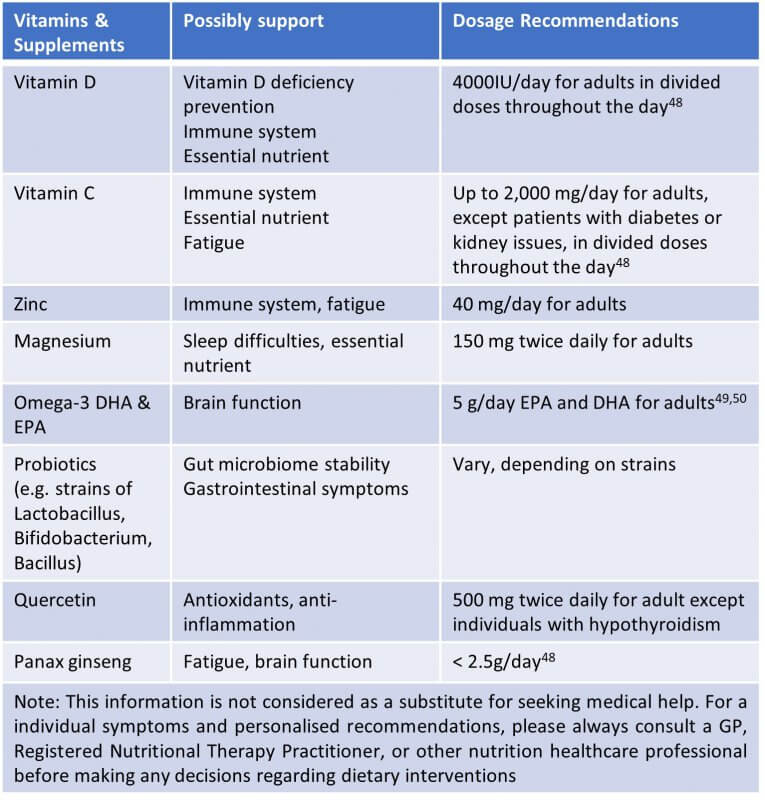
The third strategy aims to support symptoms for long hauliers with supplements supporting long-COVID symptoms. Some dietary supplements such as vitamin D, vitamin C, Zinc were highly considered to support the immune system in fighting off COVID-19 and now are thought to help with some long hauliers’ common symptoms. Few primary studies to date examined the effect of micronutrients and probiotics on fatigues, memory and cognitive dysfunction among people with long-COVID.
A small study37 found that vitamin D status is not associated with COVID-related fatigue symptoms and also reduced exercise tolerance (Townsend et al. 2021). However, we interpret the result with a limitation because two-third of participants already had an adequate vitamin D status (>50 nmol/L). Thus, the study had limited ability to detect a link between vitamin D and these symptoms. Research on supplements like vitamin D has some challenges to explore the cause-effect relationship on prevention and treatment for long-COVID. For example, there are variations in diet, lifestyle, ethnicity, and even genetic variants that can affect vitamin D status. A study 38 published in the Scientific Reports Nature journal revealed that genes such as CYP2R1, GC, and RXRA might play a role in different responses to vitamin D supplementation as well. Thus, vitamin D supplements may only be effective with some people. It is worth noting that Vitamin D is highly important for bone health and supports the immune system. Vitamin D can also regulate anti-inflammatory responses by inhibiting pro-inflammatory pathways including cytokine storm that was well-reported to COVID39. Thus, vitamin D may be a beneficial addition, particularly during winter when sunlight is limited or for individuals in whom deficiency is suspected or confirmed. A systematic review and meta-analysis found that being overweight or obese is a factor known to increase the risk of vitamin D deficiency, regardless of age and location40.
In a study41 led by Rossato (2021), around 200 people with persisting fatigue symptoms (>4 weeks) post onset of the acute phase of their COVID were supplemented with Magnesium, iron, Vitamin B3, Vitamin C, and Panax ginseng extract. As a result, 76.62% and 90.05% of participants improved their fatigue symptoms after 2 weeks and 4 weeks of the intervention, respectively (p<0.05). The fatigue improvement was measured by the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F) questionnaires. The finding published by the Clinical Nutrition ESPEN Journal is striking, but its major limitation is an open-label trial without controls. By identifying the limitation, the authors suggested a further need for more well-designed studies (e.g., RCTs) to address the cause-effect relationship.
A randomised controlled trial (RCT)42 using probiotics with strains of Bacillus in combination with systemic enzymes including bromelain demonstrated that 91% of participants in intervention groups improved fatigue symptoms in the 14-day intervention period, compared to 15% of people in the control group (Rathi et al. 2021). The authors used the Chalder fatigue scale (CFQ 11) symptom questionnaires to measure the outcome in both groups. Notably, this RCT is small and depends on self-reported data from the groups, and a short time of intervention, so any conclusions are correlational at best.
Altogether, all the dietary supplements in supporting long-COVID symptoms have been summarised in Table 1. It is worth noting that researchers are still examining the effects of vitamins and dietary supplements that work best for symptoms for COVID-19 long hauliers.
Table 1: Dietary supplements supporting post-COVID conditions
Further BANT Resources on Long-COVID
For more information and nutrition and lifestyle resources visit our website a:
- Nutrition Evidence Database (NED) Alert dedicated to COVID, Long-COVID and the latest research
- NED Infobite on Long COVID – pdf download
About the Author

Anh Nguyen is a Registered Nutritional Therapy Practitioner and certified consultant in genomic medicine who works in the intersection of nutrition and genomics to treat and prevent chronic diseases. He serves as the Chief Nutrition Consultant to Children & Women Health Service in Edinburgh. He is also a clinician-researcher at the University of Stirling, UK. His work focuses on patient-oriented research projects on precision nutrition and genomics. He is the author or co-author of peer-reviewed publications and books in the field. Most recently in the book “Complications of Pregnancy”, edited by Professor Hassan, he features pregnancy nutrition therapy for Asian women. He is also known for the efforts to explain profound concepts in personalised nutrition and lifestyle medicine between Europeans and Asians in the UK.
As of early 2021, he has been honoured as a Fellow of the British Association for Nutrition and Lifestyle Medicine at age 32. He is also elected for Ambassadorial Scholar to the Genetics Society, one of the oldest learned societies in the UK devoted to genetics, in order to promote education and research on nutritional genomics for healthcare professionals in the UK and Asia. He is a member of the Complementary and Natural Healthcare Council, the Association of Genetic Nurses and Counsellors, and the British Society of Genetic Medicine. Outside of research and practice, he currently serves as Associate Editor of the Journal Harvard Public Health Review at Harvard University.
He received an MSc in Nutritional Therapy from the University of Worcester, where he completed clinical rotations and assessments to certify as a Registered Nutrition Practitioner in the UK by the PSA through the CNHC. He then extended his studies in genomic medicine at the University of South Wales before moving to the University of Stirling for his clinical doctorate.
References
- Nasserie T., Hittle M., (2021) Goodman SN. Assessment of the Frequency and Variety of Persistent Symptoms Among Patients With COVID-19: A Systematic Review. JAMA Netw Open. 4(5):e2111417.
- Reuters (2021) English study finds long COVID affects up to 1 in 7 children months after infection
- Thomson H. (2021). Children with long covid. New scientist (1971), 249(3323), 10–11.
- Blomberg, B., et al. (2021) Long COVID in a prospective cohort of home-isolated patients. Nat Med 27, 1607–1613.
- COVID-19 Host Genetics Initiative (2021) Mapping the human genetic architecture of COVID-19. Nature.
- Dubé, MP et al. (2021) Genetics of symptom remission in outpatients with COVID-19. Sci Rep. 11, 10847
- Namkoong, H. et al. (2021) Japan COVID-19 Task Force: a nation-wide consortium to elucidate host genetics of COVID-19 pandemic in Japan. MedRxiv (preprint). 2021. Available: https://doi.org/10.1101/2021.05.17.21256513
- Alford, J. (2021) Over 2 million adults in England may have had long COVID – Imperial REACT. Accessed 24 July 2021. Available: https://www.imperial.ac.uk/news/224853/over-million-adults-england-have-long/
- Galeotti, C., Bayry, J. (2020) Autoimmune and inflammatory diseases following COVID-19. Nat Rev Rheumatol 16, 413–414.
- Matschke, J., et al. (2020). Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 19, 919–929.
- Gaebler, C. et al. (2021). Evolution of antibody immunity to SARS-CoV-2. Nature 591, 639–644.
- Khamsi, R. (2021). Rogue antibodies could be driving severe covid-19. Nature 590, 29–31.
- Halpert G., Shoenfeld Y., (2020) SARS-CoV-2, the autoimmune virus. Autoimmun Rev 19(12):102695.
- Abate SM, et al. (2021) Prevalence and outcomes of malnutrition among hospitalized COVID-19 patients: A systematic review and meta-analysis. Clin Nutr ESPEN. 43:174-183.
- Cámara, M. et al. (2021) Review of the Role of Micronutrients and Bioactive Compounds on Immune System Supporting to Fight against the COVID-19 Disease. Foods, 10, 1088.
- Wang, MX et al. (2021). Micronutrients Deficiency, Supplementation and Novel Coronavirus Infections-A Systematic Review and Meta-Analysis. Nutrients, 13(5), 1589.
- Ettman C.K., et al. (2020) Prevalence of Depression Symptoms in US Adults Before and During the COVID-19 Pandemic. JAMA Netw Open. 3(9):e2019686.
- Choi EPH, et al., (2020) Depression and Anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 17(10):3740.
- Mazza MG, et al. (2020) COVID-19 BioB Outpatient Clinic Study group, Benedetti F. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav Immun. 89:594-600.
- Taquet, M., et al. (2021) 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry, 8: 416–27
- Dimitrov S., et al. (2017) Inflammation and exercise: Inhibition of monocytic intracellular TNF production by acute exercise via β2-adrenergic activation. Brain Behav Immun. 61:60-68.
- da Silveira MP, et al. (2021) Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature. Clin Exp Med;21:1–14
- Stockwell, S., et al. (2021) Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: a systematic review. BMJ open sport & exercise medicine, 7(1), e000960.
- Okely, AD. et al. (2021) Global effect of COVID-19 pandemic on physical activity, sedentary behaviour and sleep among 3- to 5-year-old children: a longitudinal study of 14 countries. BMC Public Health 21, 940
- Sallis, R. et al. (2021) Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: A study in 48 440 adult patients. J. Sports Med.
- Stansfield, C., et al. (2016).Exploring issues in the conduct of website searching and other online sources for systematic reviews: how can we be systematic? Syst Rev 5, 191
- Doykov I, et al. (2020) The long tail of Covid-19 – The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Res, 9:1349.
- Storz, M.A. (2021) Lifestyle Adjustments in Long-COVID Management: Potential Benefits of Plant-Based Diets. Curr Nutr Rep, 1–12.
- Chen Y, et al. (2021) Six-month follow-up of gut microbiota richness in patients with COVID-19. Gut
- Carabotti M., et al. (2015) The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol, 28(2):203-209.
- Dixon Clarke S.E., Ramsay R.R. (2011) Dietary inhibitors of monoamine oxidase A. J Neural Transm (Vienna), 118(7):1031-41.
- Høier A.T.Z.B., (2021) Possibilities for Maintaining Appetite in Recovering COVID-19 Patients. Foods, 10(2):464.
- Harvard Health. Eight steps to mindful eating. Accessed 16/08/2021. Available: https://www.health.harvard.edu/staying-healthy/8-steps-to-mindful-eating
- Framson, C., et al. (2009). Development and validation of the mindful eating questionnaire. Journal of the American Dietetic Association, 109(8), 1439–1444.
- Warren J.M., et al. (2017) A structured literature review on the role of mindfulness, mindful eating and intuitive eating in changing eating behaviours: effectiveness and associated potential mechanisms. Nutrition research reviews, 30(2):272-83
- Hanh TN and Cheung L. (2012) Savor Mindful Eating Mindful Life. Harper Collin
- Townsend, L. et al. (2021). Investigating the Relationship between Vitamin D and Persistent Symptoms Following SARS-CoV-2 Infection. Nutrients, 13(7), 2430.
- Zhang, M., et al. (2017) SNP rs11185644 of RXRA gene is identified for dose-response variability to vitamin D3 supplementation: a randomized clinical trial. Sci Rep 7, 40593.
- Anh Nguyen (2020) Vitamin D and SARS-CoV-2. Swiss Medical Weekly. Available: https://smw.ch/op-eds/post/vitamin-d-and-sars-cov-2
- Pereira-Santos M, et al. (2015) Obesity and vitamin D deficiency: a systematic review and meta-analysis. Obes Rev. 16(4):341-9.
- Rossato MS, et al. (2021) Observational study on the benefit of a nutritional supplement, supporting immune function and energy metabolism, on chronic fatigue associated with the SARS-CoV-2 post-infection progress. Clinical Nutrition ESPEN.
- Rathi A, et al. (2021) A Randomized Controlled Trial of the Efficacy of Systemic Enzymes and Probiotics in the Resolution of Post-COVID Fatigue. Medicines, 8(9):47.
- Crook H, et al. (2021) Long covid-mechanisms, risk factors, and management. BMJ, 374:n1648.
- Prentiss, A. (2020) FSU Faculty gives insight on mindful eating during COVID-19. Florida State University News
- Holdoway A. (2021) Addressing nutrition in the road map of recovery for those with long COVID-19. Br J Community Nurs. 26(5):218-222.
- Bland J. S. (2020). The Long Haul of COVID-19 Recovery: Immune Rejuvenation versus Immune Support. Integrative medicine (Encinitas, Calif.), 19(6), 18–22.
- Theoharides, T. C., et al. (2021). Long-COVID syndrome-associated brain fog and chemofog: Luteolin to the rescue. BioFactors (Oxford, England), 47(2), 232–241.
- National Institute of Health (2021) Dietary Supplements in the Time of COVID-19. Fact Sheet for Health Professionals. Accessed 20 September 2021. Available: https://ods.od.nih.gov/factsheets/COVID19-HealthProfessional/
- European Food Safety Authority. (2012) scientific opinion on the tolerable upper intake level of eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA) and docosapentaenoic acid (DPA). EFSA Journal, 10:2815.
- S. Food and Drug Administration. (2019) Qualified Health Claims: Letters of Enforcement Discretion. 2019.