17 Nov 2025 The Gut-Liver-Brain Connection: How Gut Health Impacts Detoxification and Mood
The gut–liver–brain axis is a complex, bidirectional communication network linking the gastrointestinal tract, liver, and central nervous system (CNS). This set of organs plays a key role in maintaining homeostasis, influencing different physiological processes, including detoxification and mental health. Understanding these interactions is particularly important in certain age groups such as adolescents and young adults, where lifestyle choices can have lasting impacts on cognitive function, mood, and overall well-being.
 The Gut Microbiota
The Gut Microbiota
The human gastrointestinal tract hosts a diverse community of microorganisms, collectively called the gut microbiota. These microbes are vital for digestion, immune function, and neurotransmitter synthesis. Approximately 90% of the body’s serotonin, a neurotransmitter regulating mood, is produced in the gut. Dysbiosis, or microbial imbalance, is linked to mental disorders such as depression and anxiety.
The Liver and its role in Detoxification
The liver is the body’s primary detoxification organ, metabolising and eliminating internal and external toxins. It processes nutrients absorbed from the gut and filters harmful substances from the bloodstream. Impaired liver function can result in toxin accumulation, negatively affecting brain function and mood and having long-term detrimental effects on cognition.
The Brain and Central nervous system
The brain communicates with the gut and liver through neural, hormonal, and immune pathways. The vagus nerve is a major conduit for signals between the gut and brain. It runs from the brainstem down the neck into the chest and belly, connecting the brain to the heart, lungs, and digestive organs. The liver produces bile acids that influence gut microbiota composition, creating a feedback loop affecting both liver and brain health.
How diet affects the Gut–Liver–Brain Axis
The Role of Dietary Sugars
The liver is involved in glucose regulation through processes such as glycogenesis (storing glucose as glycogen), glycogenolysis (releasing glucose when needed), and glycolysis (breaking down glucose for energy). When these processes are disrupted by chronic high sugar intake, this can lead to metabolic stress on the liver and impaired detoxification capacity. Moreover, excessive sugars feed certain gut bacteria and yeasts, contributing to gut microbiota dysbiosis—an imbalance that reduces beneficial bacteria and increases intestinal permeability (or “leaky gut”). This allows bacterial endotoxins, such as lipopolysaccharides (LPS), to enter the bloodstream and reach the liver, triggering inflammation. Over time, this systemic inflammation can reach the brain, affecting neurotransmitter balance, mood, and cognitive function. High intake of added sugars, particularly from sweets, sugary drinks, pastries, and processed foods, can significantly alter the gut–liver–brain axis and lead to spikes in blood glucose and insulin, which may cause insulin resistance and fat accumulation in the liver long term.
The Role of Dietary Fats
The liver plays a central role in fat metabolism, converting dietary fats, carbohydrates, and proteins into energy substrates, making cholesterol and bile acids necessary for digestion. While excessive intake of saturated and trans fats, found in fatty meats, butter, processed snacks, and fried foods, can contribute to inflammation and stress on the liver, not all fats have the same effects. The balance between saturated and unsaturated fats appears to be key point in supporting metabolic, hepatic, and cognitive health. Some guidelines advise limiting saturated fats to no more than 10% of total energy intake. Diets high in both saturated fats and refined sugars, may lead to hepatic fat accumulation which on another hand may cause non-alcoholic fatty liver disease (NAFLD) and impaired detoxification capacity. Conversely, unsaturated fats, particularly omega-3 fatty acids from oily fish (such as salmon, sardines, and mackerel), walnuts, flaxseeds, and chia seeds, have powerful anti-inflammatory and neuroprotective effects. These essential fatty acids (EFAs) help regulate cytokine production, small signalling proteins that control inflammation, while preserving cell membrane fluidity and supporting neurotransmitter synthesis. Some evidence suggests that maintaining a dietary ratio of omega-6 to omega-3 fats between approximately 1: 1 and 4 : 1 is optimal for health, compared with ratios exceeding 15: 1 typically seen in Western diets. Excessive omega-6 fatty acids, mainly found in processed seed oils such as sunflower, soybean, and corn oil, can promote a pro-inflammatory environment, whereas omega-3s help restore immune balance and support gut barrier integrity. Balanced saturated-to-unsaturated fat ratio, alongside reduced refined carbohydrate intake, stimulates hepatic lipid metabolism and may reduce systemic inflammation. Diets rich in monounsaturated and polyunsaturated fats, such as those following a Mediterranean-style pattern, have been shown to lower liver fat accumulation, improve insulin sensitivity, and promote a more diverse gut microbiota (Mascaró, Bouzas and Tur, 2022).Emerging research also highlights that whole-food ketogenic or low-carbohydrate diets, when based on unsaturated fats and nutrient-dense ingredients, may reduce oxidative stress and improve hepatic mitochondrial efficiency (Luukkonen et al., 2020) . These dietary approaches, when carefully implemented, can enhance metabolic flexibility and stabilise blood glucose, thereby supporting the gut–liver–brain axis and promoting both detoxification and cognitive resilience.
· Low-Fibre Diets – Low dietary fibre reduces the production of short-chain fatty acids (SCFAs), which are critical for gut barrier integrity and inflammation modulation. SCFA deficiencies may compromise gut health and cognitive function.
· Fermented Foods- Fermented foods enhance gut microbial diversity and produce beneficial metabolites. Probiotics from foods such as kimchi, miso, and kefir can reduce anxiety and depressive symptoms.
Detoxification and Mood Regulation
The liver is the body’s primary detoxification organ, responsible for metabolising endogenous and exogenous compounds, including drugs, environmental toxins, and metabolic by-products. Efficient detoxification is critical not only for physical health but also for mental well-being. Impairments in liver function can trigger a cascade of physiological changes that directly impact the brain, contributing to mood disorders, cognitive impairments, and overall mental fatigue.
Toxin Accumulation and Neurotransmitter Disruption
When liver function is compromised—due to poor diet, genetic predisposition, or exposure to environmental toxins—metabolic by-products such as ammonia, homocysteine, and bile acid derivatives can accumulate in the bloodstream. These compounds can cross the blood-brain barrier influencing neurotransmitter synthesis and signalling pathways. For example, elevated ammonia levels interfere with glutamate and GABA neurotransmission, contributing to anxiety, irritability, and cognitive disturbances.
Similarly, impaired liver metabolism can alter the availability of tryptophan, a precursor to serotonin, reducing mood-stabilising neurotransmitters and increasing the risk of depression. Chronic exposure to systemic toxins also triggers oxidative stress and inflammation in the CNS, further disrupting neurotransmission and neuronal health.
Inflammation and Gut-Derived Endotoxins
The gut–liver–brain axis is highly sensitive to inflammation. Dysbiosis, or microbial imbalance, can increase intestinal permeability (“leaky gut”), allowing lipopolysaccharides (LPS) and other bacterial endotoxins to enter the digestive circulation and reach the liver. The liver responds by releasing inflammatory substances called cytokines into systemic circulation. These cytokines can cross into the brain, promoting neuroinflammation, which has been implicated in the pathophysiology of depression, anxiety, and impaired cognitive function.
Environmental toxins—such as heavy metals, pesticides, and air pollutants—can compound this effect overwhelming the liver’s detoxification capacity and increasing systemic inflammation. This is particularly concerning in modern urban environments, where exposure to multiple pollutants in big cities is common.
Oxidative Stress and Mitochondrial Dysfunction
Detoxification processes in the liver, particularly Phase I metabolism, generate reactive oxygen species (ROS) as by-products. Normally, antioxidants such as glutathione neutralise ROS. However, when liver function is impaired or antioxidant stores are depleted, ROS accumulate, causing oxidative stress that can damage liver cells and brain neurons alike. Mitochondrial dysfunction in neurons, impairs energy production, leading to fatigue, poor concentration, and mood instability.
What are the clinical implications
Several studies demonstrate a strong link between liver dysfunction and mental health disorders. Individuals with non-alcoholic fatty liver disease (NAFLD) are more likely to experience depression and anxiety, independent of other metabolic conditions. Similarly, adolescents and young adults with impaired liver detoxification due to poor dietary habits, alcohol consumption, or disordered eating are at heightened risk for mood swings, reduced academic performance, and cognitive deficits.
Understanding this connection highlights the importance of supporting liver health not just for physical detoxification but also as a foundational strategy for mental well-being. Nutritional support, lifestyle modifications, and early interventions targeting gut–liver–brain health can help reduce neuroinflammation, improve neurotransmitter balance, and optimise cognitive function.
Supporting Detoxification for Mental Health
- Optimise Antioxidant Intake: Foods rich in vitamin C, E, polyphenols, and selenium help neutralise ROS generated during detoxification.
- Enhance Glutathione Production: N-acetylcysteine (NAC), cruciferous vegetables, and proteins can support glutathione synthesis.
- Promote Healthy Gut Barrier: Prebiotics, probiotics, and high-fibre diets reduce endotoxin leakage from the gut.
- Minimise Exposure to Toxins: Limit alcohol, avoid smoking, and reduce exposure to environmental pollutants.
- Support Liver Enzymatic Function: Adequate protein, B vitamins, and choline-rich foods enhance Phase I and Phase II detoxification pathways.
Nutrition and Supplements to Support Liver Function
Certain nutrients are proven in supporting liver function and optimising detoxification.
- Choline: Essential for the export of fat from the liver, helping to prevent fat accumulation and supporting brain function. Good sources include eggs, lean chicken, salmon, and Brussels sprouts.
- Methionine: Supports methylation pathways, which are critical for detoxification and the synthesis of neurotransmitters. Rich sources include turkey, fish, sesame seeds, and lentils.
- Antioxidant Vitamins: Vitamins C, E, and A protect liver cells from oxidative damage, supporting detoxification and overall metabolic health. Vitamin C can be found in high concentrations in oranges, kiwis, and bell peppers and generally found in all fruits and vegetables; vitamin E in almonds, sunflower seeds, and spinach; and vitamin A in carrots, sweet potatoes, and liver.
- Minerals: Zinc, selenium, and magnesium assist liver enzyme function and help reduce inflammation. Zinc is abundantly found in oysters, beef, and pumpkin seeds; selenium in Brazil nuts, tuna, and eggs; and magnesium in spinach, almonds, and whole grains.
Foods for Liver Support
- Polyphenol-rich foods: Berries, green tea, and cruciferous vegetables such as broccoli, cabbage, cauliflower, Brussel sprouts, enhance liver detoxification enzymes and bile production.
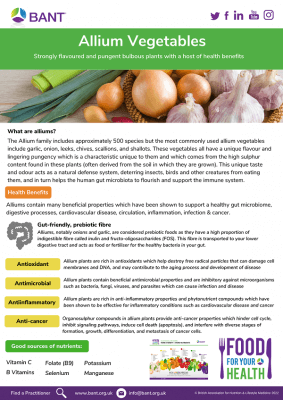
- Allium vegetables: Garlic and onions contain organosulfur compounds that stimulate phase II liver detoxification.
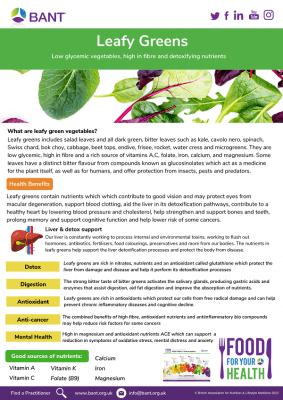
- Leafy greens: Spinach, kale, and dandelion support bile flow and antioxidant capacity making these foods great choice for everyday liver support.
Nutritional Supplements
- Milk thistle (silymarin): Promotes liver cell regeneration and reduces inflammation.
- N-acetylcysteine (NAC): Boosts glutathione production, a major intracellular antioxidant protecting liver cells.
- Omega-3 fatty acids: Improve hepatic lipid metabolism and reduce fatty liver accumulation.
- Vitamin B complex: Supports methylation pathways and detoxification processes which may also support with energy levels.
While supplements can offer additional support, a nutrient-dense, whole-food diet remains the foundation for liver and brain health.
The Gut–Liver–Brain Axis in Teens and Young Adults
Adolescence and early adulthood are critical phases for brain and liver development, during which lifestyle and dietary habits can shape long-term cognitive, emotional, and metabolic health. The gut–liver–brain axis is particularly influential at this stage; imbalance in one system can disrupt the others, contributing to persistent physiological and psychological effects.In the UK, the rise in youth mental health concerns has been striking. The NHS found that 20.3% of children aged 8–16 and 23.3% of those aged 17–19 had a probable mental disorder, rising to 21.7% among 20–25-year-olds. Rates were notably higher in young women (31.6%) than men (15.4%). Similarly, research by the Mental Health Foundation reported that 27% of British teenagers felt “nervous, anxious or on edge” ,while 32% struggled with sleep.
This escalating mental health burden coincides with increasing consumption of ultra-processed foods, irregular sleep patterns, academic pressure, and social media exposure, all factors known to disrupt gut microbial diversity, liver metabolism, and neurotransmitter balance.
Dietary Patterns and Nutrient Intake
Teens and young adults are increasingly exposed to diets high in ultra-processed foods, refined sugars, and saturated fats, often coupled with low intake of fibre, fresh vegetables, and essential nutrients. Research shows that diets high in sugar and trans fats are associated with altered gut microbiota composition, reduced production of beneficial short-chain fatty acids (SCFAs), and increased systemic inflammation. These dietary patterns can contribute to non-alcoholic fatty liver disease (NAFLD), impair detoxification, and negatively impact neurotransmitter synthesis, particularly serotonin and dopamine, which are essential for mood, motivation, and learning.
Key nutrient deficiencies commonly observed in adolescents, such as vitamin B12, folate, iron, and omega-3 fatty acids, are linked to cognitive deficits, reduced memory performance, and mood disturbances. Ensuring adequate intake of these nutrients through balanced meals or supplementation is critical for maintaining both liver and brain function during these early years.
Disordered Eating and Body Image
Disordered eating behaviours, such as restrictive dieting, binge eating, and meal skipping, are increasingly common among UK adolescents and young adults, particularly those heavily exposed to social media influence. According to NHS, around 12% of 17–19-year-olds in England screened positive for a possible eating disorder, more than double the 2017 figure. Meanwhile, Beat Eating Disorders (2024) estimates that 1.25 million people in the UK are currently affected, with adolescents and young adults most at risk. Concerns about body image also remain widespread: 40% of teenage girls and 23% of boys report dissatisfaction with their appearance (Mental Health Foundation,2023). Such behaviours impose metabolic and psychological strain by impairing nutrient metabolism, increasing oxidative stress, and disrupting gut microbiota balance. Restrictive diets may limit intake of nutrients vital for liver detoxification, such as choline, methionine, and B vitamins, while binge eating may trigger hepatic fat accumulation and systemic inflammation. These disruptions in eating habits may compromise the gut–liver–brain axis, affecting mood regulation, concentration, and cognitive function. Early nutrition education and supportive community environments can help reduce disordered eating behaviours and prevent long-term physical and psychological risks.
Substance Use and Environmental Factors
Alcohol, recreational drug use, and environmental toxins pose additional threats to the gut–liver–brain axis in young people. Despite a gradual decline in underage drinking, alcohol remains widely used. The NHS reports that 45% of 17–24-year-olds had consumed alcohol, with binge drinking more common in young men. Even moderate consumption during adolescence can increase intestinal permeability and systemic inflammation, placing strain on both the liver and brain. Recreational drug use adds further risk. The Office for National Statistics (2024) found that 18.5% of 16–24-year-olds had used illicit drugs in the past year, most commonly cannabis (15.5%), followed by nitrous oxide and cocaine. Prolonged use is linked to dysbiosis, impaired nutrient absorption, and hepatic mitochondrial dysfunction, all of which can negatively affect cognitive and emotional regulation.
Environmental pollutants further compound these challenges. Young people are increasingly exposed to endocrine-disrupting chemicals, heavy metals, and microplastics via diet, air, and water. Evidence reviewed by Public Health England (2022) highlights the growing burden of environmental toxins on metabolic and neurological health, with links to oxidative stress, reduced detoxification capacity, and altered liver enzyme activity.
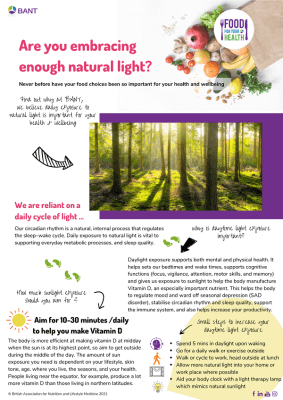
Academic Stress, Sleep, and Lifestyle
Adolescents and young adults face unique lifestyle pressures, including academic demands, irregular sleep patterns, and high screen time. Chronic stress activates the hypothalamic–pituitary–adrenal (HPA) axis, increasing cortisol levels, which in turn can alter gut microbiota composition and impair liver detoxification processes. Sleep deprivation, common in this age group, negatively impacts the circadian rhythms (sleep pattern) that regulate liver metabolism, bile acid production, and neurotransmitter synthesis, further affecting mood, attention, and learning capacity.
Supporting Gut–Liver–Brain Health in Teens and Young Adults
Effective strategies to support this axis in young populations involve a combination of nutrition, lifestyle modification, and early intervention:
- Balanced Diet: Emphasise whole foods, high-fibre fruits, vegetables, lean proteins, and omega-3-rich sources like oily fish, flaxseeds, and walnuts.
- Meal Timing and Regularity: Avoid skipping meals to prevent liver metabolic stress and maintain stable neurotransmitter production.
- Probiotics and Fermented Foods: Encourage fermented foods such as yogurt, kefir, kimchi, or miso to promote gut microbiota diversity.
- Hydration: Adequate water intake supports liver detoxification and metabolic function.
- Sleep Hygiene: Prioritising 7–9 hours of sleep per night helps maintain liver metabolism and brain function.
- Stress Management: Mindfulness, yoga, deep-breathing exercises, and moderate exercise reduce HPA axis activation and support gut–brain communication.
- Moderate Alcohol and Avoid Drugs: Limiting exposure protects both liver function and cognitive performance.
- Early Screening and Support: Monitoring for disordered eating, mental health challenges, or liver function markers allows for early intervention and lifestyle guidance.
Conclusion
The gut–liver–brain axis is central to detoxification, cognitive function, and mental health. Optimising this axis through dietary strategies, functional foods, supplements, and lifestyle interventions is crucial — especially for adolescents and young adults exposed to poor diets, environmental toxins, and lifestyle stressors. By supporting gut and liver health, individuals can enhance mood regulation, memory, and overall wellbeing.
It would be great to have some current UK stats on Teen mental heath
Author: Simona Yakarova, BANT Registered Nutritionist®

REFERENCES:
- Air pollution: applying All Our Health (2022). https://www.gov.uk/government/publications/air-pollution-applying-all-our-health/air-pollution-applying-all-our-health.
- Alberti, K.G.M.M. et al. (2009) ‘Harmonizing the metabolic syndrome’, Circulation, 120(16), pp. 1640–1645. doi:10.1161/circulationaha.109.192644.
- Beat Eating Disorders (2024) Statistics on Eating Disorders in the UK. Available at: https://www.beateatingdisorders.org.uk
- Bordoni, L. et al. (2025) Editorial: The role of dietary fatty acids in metabolic health, Frontiers. Available at: https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2023.1211151/full
- Calderon Martinez, E. et al. (2023) ‘Impact of silymarin supplements on liver enzyme levels: A systematic review’, Cureus [Preprint]. doi:10.7759/cureus.47608.
- Di Vincenzo, F. et al. (2023) ‘Gut microbiota, intestinal permeability, and systemic inflammation: A narrative review’, Internal and Emergency Medicine, 19(2), pp. 275–293. doi:10.1007/s11739-023-03374-w.
- Gibson, G., Hutkins, R., Sanders, M. et al. Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nat Rev Gastroenterol Hepatol 14, 491–502 (2017). https://doi.org/10.1038/nrgastro.2017.75
- Guan, Y.-S. and He, Q. (2015) ‘Plants consumption and liver health’, Evidence-Based Complementary and Alternative Medicine, 2015, pp. 1–10. doi:10.1155/2015/824185.
- Heindel, J.J. et al. (2017) ‘Metabolism disrupting chemicals and metabolic disorders’, Reproductive Toxicology, 68, pp. 3–33. doi:10.1016/j.reprotox.2016.10.001.
- Hodges, R.E. and Minich, D.M. (2015) ‘Modulation of metabolic detoxification pathways using foods and food-derived components: A scientific review with Clinical Application’, Journal of Nutrition and Metabolism, 2015, pp. 1–23. doi:10.1155/2015/760689.
- Köck, P., Meyer, M., Elsner, J., Dürsteler, K.M., Vogel, M. and Walter, M. (2022). Co-occurring Mental Disorders in Transitional Aged Youth With Substance Use Disorders – A Narrative Review. Frontiers in Psychiatry, 13. doi:https://doi.org/10.3389/fpsyt.2022.827658.
- Li, Z., et al. (2020) ‘Methionine metabolism and liver disease’, Signal Transduction and Targeted Therapy, 5, 241. doi:10.1038/s41392-020-00349-7.
- Lepretti, M., Martucciello, S., Burgos Aceves, M. A., Putti, R., and Lionetti, L. (2018). Omega-3 fatty acids and insulin resistance: Focus on the regulation of mitochondria and endoplasmic reticulum stress. Nutrients 10, 350. doi:10.3390/nu10030350
- Luukkonen, P. K., Sadevirta, S., Zhou, Y., Kayser, B., Ali, A., Ahonen, L., et al. (2018). Saturated fat is more metabolically harmful for the human liver than unsaturated fat or simple sugars. Diabetes Care 41, 1732–1739. doi:10.2337/dc18-0071
- Luukkonen, P.K. et al. (2020) ‘Effect of a ketogenic diet on hepatic steatosis and hepatic mitochondrial metabolism in nonalcoholic fatty liver disease’, Proceedings of the National Academy of Sciences, 117(13), pp. 7347–7354. doi:10.1073/pnas.1922344117.
- Mascaró, C.M., Bouzas, C. and Tur, J.A. (2022). Association between Non-Alcoholic Fatty Liver Disease and Mediterranean Lifestyle: A Systematic Review. Nutrients, [online] 14(1), p.49. doi:https://doi.org/10.3390/nu14010049.
- Mehedint, M.G. and Zeisel, S.H. (2013) ‘Cholineʼs role in maintaining liver function’, Current Opinion in Clinical Nutrition and Metabolic Care, 16(3), pp. 339–345. doi:10.1097/mco.0b013e3283600d46.
- Mental Health Foundation. (2022). Teenagers’ mental health under severe pressure as pandemic continues – new research. [online] Available at: https://www.mentalhealth.org.uk/about-us/news/teenagers-mental-health-under-severe-pressure-pandemic-continues-new-research?utm_source
- Mental Health Foundation (2023). Body image report: Introduction. [online] www.mentalhealth.org.uk. Available at: https://www.mentalhealth.org.uk/our-work/research/body-image-how-we-think-and-feel-about-our-bodies/body-image-report-introduction.
- NHS (2023) Mental health of children and young people in England, 2023: Wave 4 follow up to the 2017 survey. Part 1: Mental health. [Online] Available at: https://digital.nhs.uk/data-and-information/publications/statistical/mental-health-of-children-and-young-people-in-england/2023-wave-4-follow-up/part-1-mental-health
- NHS (2024). Health Survey for England – NHS Digital. [online] NHS Digital. Available at: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england.
- Nikbaf-Shandiz, M. et al. (2023) ‘The efficacy of N-acetylcysteine in improving liver function: A systematic review and meta-analysis of controlled clinical trials’, PharmaNutrition, 24, p. 100343. doi:10.1016/j.phanu.2023.100343.
- Office for National Statistics (ONS) (2024) Drug misuse in England and Wales: year ending June 2024. [Online] Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/drugmisuseinenglandandwales/yearendingmarch2024
- Piotr Służały, Paweł Paśko and Galanty, A. (2024). Natural Products as Hepatoprotective Agents—A Comprehensive Review of Clinical Trials. Plants, [online] 13(14), pp.1985–1985. doi:https://doi.org/10.3390/plants13141985.
- Rizzo, M., Colletti, A., Penson, P.E., Katsiki, N., Mikhailidis, D.P., Toth, P.P., Gouni-Berthold, I., Mancini, J., Marais, D., Moriarty, P., Ruscica, M., Sahebkar, A., Vinereanu, D., Cicero, A.F.G., Banach, M., Acosta, J., Al-Khnifsawi, M., Alnouri, F., Amar, F. and Atanasov, A.G. (2023). Nutraceutical approaches to non-alcoholic fatty liver disease (NAFLD): A position paper from the International Lipid Expert Panel (ILEP). Pharmacological Research, [online] 189, p.106679. doi:https://doi.org/10.1016/j.phrs.2023.106679.
- Simopoulos, A.P. (2008) ‘The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases’, Experimental Biology and Medicine, 233(6), pp. 674–688. doi:10.3181/0711-mr-311.
- Simopoulos, A.P. (2011) ‘Evolutionary aspects of Diet: The omega-6/omega-3 ratio and the brain’, Molecular Neurobiology, 44(2), pp. 203–215. doi:10.1007/s12035-010-8162-0.
NOTES TO EDITORS:
BANT is the leading professional body for Registered Nutritional Therapy Practitioners in one-to-one clinical practice and a self-regulator for BANT Registered Nutritionists®. BANT members combine a network approach to complex systems, incorporating the latest science from genetic, epigenetic, diet and nutrition research to inform individualised recommendations. BANT oversees the activities, training and Continuing Professional Development (CPD) of its members.
Registered Nutritional Therapists are regulated by the Complementary and Natural Healthcare Council (CNHC) that holds an Accredited Voluntary Register (AVR) for the Professional Standards Authority for Health and Social Care (PSA). A report by the Royal Society for Public Health and the Professional Standards Agency made a key recommendation that AVR practitioners have the authority to make direct NHS referrals, in appropriate cases, to ease the administrative burden on GP surgeries. BANT nutrition practitioners are the key workforce asset to harness 21st-century lifestyle medicine to tackle the rising tide of stress-related fatigue, obesity, Type 2 Diabetes, dementia and other chronic diseases.
To find a BANT nutrition practitioner, please click here
BANT WELLBEING GUIDELINES:
The BANT Wellbeing Guidelines are specifically designed to provide clear, easy-to-understand general information for healthy diet and lifestyle when personalised advice is not available.
Alongside these guidelines, the BANT “Food for your Health” free open-access resources are available to educate and guide the public towards healthier food choices in the prevention of diet-induced disease. Download a wide range of food and lifestyle guides, recipes, infographics, planning tools and fact sheets and start making healthy choices today.